News
Tirzepatide Prescribing
From 23 June 2025, people living with obesity and four or more diagnosed health conditions will begin to have the opportunity to access tirzepatide (Mounjaro®) for weight loss support through their GP /Primary Care services. This process will be managed through the practice directly contacting people who are eligible, this does not mean that prescriptions will be given out immediately. Practices will be contacting people who have been identified as eligible over the coming weeks.
Access to the medication goes hand in hand with support to help with eating habits and start/improve physical activity as part of a national wrap around service. Access to prescribed weight loss medication will be predicated on a patients engagement with this service.
At NHS Sussex, we are committed to helping people live healthier lives. We understand how difficult it can be for many people living with obesity to access the support they need. That is why we are working closely with partners across Sussex to provide services that help people make long-term, sustainable changes to improve their wellbeing.
Obesity is a complex health condition and one of the leading contributors to serious illnesses such as cardiovascular disease, type 2 diabetes and some forms of cancer. It also places a significant strain on health services, costing the NHS around £6.5 billion each year.
Full qualifying criteria is a BMI (Body Mass Index) of 40 or greater and four or more of the
following diagnosed health conditions:
• type 2 diabetes
• Hypertension
• Cardiovascular disease
• Obstructive sleep apnoea
• Dyslipidaemia
We understand that some people may feel frustrated or disappointed if they are not eligible for medication-based treatments at this stage. Living with obesity can be emotionally and physically challenging, and it is completely normal to experience a range of feelings when seeking support for your health. If you are finding things difficult, NHS Talking Therapies offers free and confidential help for people who may be struggling with low mood, anxiety or other emotional pressures.
To find out more about obesity treatment and the support available on the NHS Sussex website: Support to manage your weight
You can also learn more about local by speaking to your GP or healthcare team.
You can also read the following for more information:
• NHS England » Weight management injections
NHS England has published a set of FAQs in relation to Mounjaro. PRN01728_Expanding Access to the Weight Loss Drug Tirzepatide - FAQs_December 2024_ Final 5.12.24.docx
On behalf of NHS Sussex


New vaccination !! RSV
The new RSV vaccine for older adults
From 1 September 2024, those who turn 75 and those age 75 to 79 will be eligible for a free vaccine to protect them from respiratory syncytial virus (RSV).
RSV is an infectious disease of the airways and lungs. RSV infection often causes symptoms similar to a cold, including:
- cough
- sore throat
- sneezing
- a runny or blocked nose
It can also make you become wheezy or short of breath and lead to pneumonia and other life-threatening conditions. There is no specific treatment, and most infections will get better by themselves. Every year thousands of older adults need hospital care for RSV, and some of them will die. RSV can be more severe in people with medical conditions such as heart or lung disease or a weakened immune system.
RSV infection is common in young children but is most serious for small babies and for older people.
There is no need to contact the practice to book. We will contact YOU when the vaccine is available and when we have clinics on to deliver this.
How RSV is spread
RSV infections can occur all year round but cases peak every winter.
RSV can spread through coughs and sneezes. You can help to prevent the spread of the virus by covering your mouth and nose when you cough or sneeze (ideally with a tissue, or else into the bend of your elbow), and you can wash your hands frequently to reduce the risk of picking up the virus. Even with these measures it can be difficult to avoid RSV infection.
The best way to protect yourself is to have the vaccine.
How the RSV vaccine works
Almost all older adults will have had several RSV infections during their life. A single dose of vaccine will help to boost protection as you reach an age group at highest risk of serious RSV infection. Unlike the flu vaccine you do not need to have the RSV vaccine every year.
Eligibility for the RSV vaccination
Everyone turning 75 years old on or after the 1 September 2024 will be offered a single dose of RSV vaccine. This is because older adults are more at risk of serious complications from RSV. You can still get the vaccine up to the day before you turn 80.
For the first year of the programme, the vaccine will also be offered to those who are already aged 75 to 79 years on 1 September 2024 as part of a catch up programme.
If you are not yet 75 the NHS will invite you for vaccination once you turn 75.
Having the RSV vaccine at the same time as other vaccines
Shingles and pneumococcal vaccines
You may be offered your shingles or pneumococcal vaccine at the same time as the RSV vaccine, it is safe to do so and reduces the number of appointments you will need to get protected from these diseases.
Flu and COVID-19 vaccines
RSV isn’t normally arranged to be given at the same appointment as your COVID-19 or flu vaccines.
In certain clinical circumstances, your doctor or nurse can safely offer them at the same time.
Those who should not have the RSV vaccine
Almost everybody can have the vaccine, but tell the doctor or nurse if you have ever had a serious allergy to a vaccine, or any of the ingredients.
You can read the patient information leaflet for the RSV vaccine called Abrysvo.
If you have a minor illness such as a cold you can receive the vaccine, but if you are very unwell or have a fever, the doctor or nurse may advise you to wait until you are better.
The protection offered by the RSV vaccine
The vaccine has been shown to reduce the chance of you suffering from RSV disease. As with all medicines, no vaccine is completely effective and some people may still get RSV despite having a vaccination. If you do get RSV, it should be less severe.
How long the RSV vaccine will protect you for
In the clinical studies, RSV vaccine provided good protection for at least 2 years and is expected to last longer.
Side effects from the RSV vaccine
You may get some soreness, redness or swelling at the site of the injection for a day or two after the vaccination.
In the first season of use in the US over 3 million doses were given. A nervous system condition that leads to weakness was reported, around 5 cases for every million doses given. The same condition also occurs after a number of common infections and some vaccines but overall it is safer for you to have the vaccine than to risk having a potentially serious RSV infection.
Further information
If you have further questions, speak to your practice nurse.
Read the patient information leaflet for the RSV vaccine Abrysvo.
Infected Blood Inquiry
Following recent media coverage about the Infected Blood Inquiry, we understand that some people may be concerned about their own health.
Please see the dedicated NHS webpage for key information about this and signposting on where to find support: https://nhs.uk/infected-blood-support
Since 1991, all blood donated in the UK is screened and distributed by NHS Blood and Transplant following rigorous safety standards and testing to protect both donors and patients.
Since testing has been introduced, the risk of getting an infection from a blood transfusion or blood products is very low.
All blood donors are screened at every donation and every donation is tested before it is sent to hospitals. Blood services and blood safety has been transformed, not only in terms of technological advances in testing but also in the way donors are recruited and checked they are safe to donate.
Given the time that has elapsed since the last use of infected blood products, most of those who were directly affected have been identified and started appropriate treatment. However, there may be a small number of patients where this is not the case, and particularly where they are living with asymptomatic hepatitis C. If you are worried about risk of hepatitis C, you can order a confidential test online through the NHS website: http://hepctest.nhs.uk.
Patients who want more details about the safety of blood from donations in England can find more information here: https://www.blood.co.uk/the-donation-process/further-information/your-safety/

Dispensary telephone lines
From 10th December 2023 our dispensary telephone line opening hours will be changing. The phone line will only be available for urgent queries, between 10:30AM-11:30AM & 15:30PM-16:30PM for patients who are housebound or have no internet access.
Blood test appointments
Due to staff shortages and insufficient funding for blood tests we need to encourage our patients that they only book blood test appoints at the surgery if the test was requested by a clinician at the surgery.
With hospital forms please book your follow up blood test appointment with the requesting organisation. E.g. St Richards Hospital.


Important information for patients currently on hospital waiting lists
The NHS has been working hard to address the backlogs built up during the COVID pandemic. As part of these plans, the NHS will be proactively contacting patients who have been waiting a long time for NHS funded treatment to remind them of their right to request to move to an alternative hospital where they may be seen quicker.
From Tuesday 31st October new digital portal called the Patient Initiated Digital Mutual Aid System (PIDMAS) will be introduced. Patients who have been waiting 40 weeks or more can use this portal to request an alternative choice of hospital.
Any patient who is eligible will receive either a SMS text message or a letter from their current hospital explaining how to request to choose a different hospital.
Please do not contact the practice regarding this process as we have no information regarding individual patients. The hospital will contact you if you are eligible. Please do not contact them either.
Further information about alternative choice is available on hospital websites.
General Practice Data for Planning and Research (GPDPR)
NHS Digital has been collecting data from GPs through its trusted General Practice Extraction Service. This system is now being replaced from 1.9.21 with their new General Practice Data for Planning and Research (GPDPR) service, a broader general-purpose collection which will enable faster access to pseudonymised patient data for planners and researchers.
This more sophisticated extraction service will be working on things such as researching the long-term impact of coronavirus on the population, analyzing healthcare inequalities and researching and developing cures for serious illnesses.
NHS Digital will collect:
- data about diagnoses, symptoms, observations, test results, medications, allergies, immunisations, referrals, recalls and appointments, including information about physical, mental and sexual health
- data on sex, ethnicity and sexual orientation
- data about staff who have treated patients
NHS Digital does not collect:
- name and address (except for postcode, protected in a unique coded form)
- written notes (free text), such as the details of conversations with doctors and nurses
- images, letters and documents
- coded data that is not needed due to its age – for example medication, referral and appointment data that is over 10 years old
- coded data that GPs are not permitted to share by law – for example certain codes about IVF treatment, and certain information about gender re-assignment
Patients can opt-out from NHS Digital COLLECTING their data (called a type 1 opt out) or dissent to NHS digital SHARING their data for planning and research (called a National data opt out). If you wish to find more information about GPDPR including your right to opt out then please follow this link https://www.nhs.uk/your-nhs-data-matters/.
You are able to opt our of GPDPR by clicking on the following link Make your choice about sharing data from your health records.
Data collection will start on 1 July 2021, if you do not want your data shared with NHS Digital this should be done by returning the form below to your GP practice by 23 June 2021 to allow time for processing it. You can send the form by post or email to your GP practice.
You can read the General Practice Data for Planning and Research: NHS Digital Transparency Notice HERE.
Alzheimer’s Society countywide continuous to offer to support Carers and People Affected by Dementia during the COVID19 pandemic.
All group activities service users are receiving regular welfare checks and connected via the delivery of virtual groups where possible.
The Dementia Advisors/Support Workers are providing welfare checks with their current caseload and telephone assessments with all new referrals. Those who are considered most vulnerable are being prioritised and referred into the relevant services.
Companion Calls are also a great new interim service that joins up our service users with a volunteer for a friendly chat. People are being devastated by isolation and loneliness right now and these calls will really help.
Locally, their ask is that people phone them for any support they need throughout the outbreak as they have a full team of home based staff and volunteers available at present. Make contact via Sussex.Helpline@alzheimers.org.uk / 01403 213017 and they will respond as soon as possible.
The Dementia Connect Support Line remains open on 0333 150 3456 every day. Dementia Talking Point, their online community, where people affected by dementia can receive valuable support, can be accessed online for free, night or day, through their website www.alzheimers.org.uk

Vitamin D Supplements Information for patients
Why is Vitamin D important?
Vitamin D is a hormone made in our bodies in the presence of sunlight. It is also found in small amounts in foods. Vitamin D is essential for bone and muscle health, and supports a healthy immune system.
Do I need to take Vitamin D supplements?
During winter, and ideally all year round, children from one year old and adults in the UK should take a daily supplement containing at least 400 international units (IU) of Vitamin D. This is equivalent to 10 micrograms (μg).
This is because there is not enough sunlight in the UK during winter (October to March) for the body to make its own Vitamin D. Whilst Vitamin D is in some foods, it is difficult for most people to get enough from food alone.
Many people do not get enough vitamin D from sunlight, even during the summer, because they have little or no sunshine exposure, or a reduced ability to make Vitamin D.
You should take a daily supplement containing at least 400 IU (10 micrograms) of Vitamin D all year round, if one or more of the following applies to you:
- You are shielding due to Covid-19
- You wear clothes that cover up most of the skin when outdoors
- You are housebound, work indoors during the day, or are a night shift worker
- You have darker skin, for example of African, African-Caribbean, Asian or Middle-Eastern descent
- You are over the age of 65
- You are pregnant or breastfeeding
Infants and children under four, who are taking less than 500ml of infant formula a day should also take 340-400 IU (8.5-10 micrograms) of Vitamin D per day, and may be eligible for free supplements on the Healthy Start Scheme.
Is it possible to take too much Vitamin D?
Some supplements contain a higher dose, such as 800 IU (20 micrograms). These are also safe and effective. However, taking more than 4000 IU (100 micrograms) of Vitamin D a day for a long time could be harmful. If you have purchased supplements containing a higher dose than this, take them less frequently so your overall intake is lower. Children under 10 should not take more than 2000 IU (50 micrograms) per day.
Will taking Vitamin D supplements help prevent Covid-19?
The direct link between Vitamin D and Covid-19 prevention and treatment is still being established.
Approved by Surrey Heartlands MM Cell Surrey Heartlands MMT Version 2 23 December 2020
Is there Vitamin D in my existing medications?
Vitamin D is often contained in calcium supplements, because the body needs Vitamin D to absorb calcium. ‘One a Day’ Multivitamin and Mineral supplements, and some Oral Nutritional Supplements also contain Vitamin D at the recommended amount, so if you take any of these, you may already be getting enough Vitamin D. If you are unsure, check with your pharmacist.
Can I get free or prescribed vitamin D?
Vitamin D is not routinely prescribed. This is because supplements are widely available to buy.
Those who have been advised to shield due to Covid-19 may be at risk of Vitamin D deficiency if they have spent little time outdoors. Therefore, in January 2021, The UK Government will deliver four months’ supply of Vitamin D supplements to those who are extremely clinically vulnerable to Covid-19.
If you are eligible, you will have received a letter inviting you to opt-in to receive the supplements. If you think you are eligible and haven’t received a letter, you can opt in by visiting The NHS website - NHS (www.nhs.uk) and typing ‘get Vitamin D’ into the search bar.
Vitamin D can be prescribed in higher doses for people who have persistent symptoms suggesting Vitamin D deficiency, which is confirmed by a blood test. Unless you have symptoms of Vitamin D deficiency you do not need to be tested, as meeting the recommended intake every day is usually enough to maintain adequate Vitamin D levels.
Which supplement should I buy?
Supplements containing 400 IU (10 micrograms) are available to purchase from pharmacies, supermarkets and online. Vitamin D is available in two forms, vitamin D3 (colecalciferol), and vitamin D2 (ergocalciferol). Vitamin D3 is usually from animal sources, and vitamin D2 is from plant sources.
My relative lives in a care home, how do they get Vitamin D supplements?
In January 2021, the UK Government will deliver four months’ supply of Vitamin D supplements to all care home residents. Residents do not need to opt in and these will be supplied automatically.
Where can I find out more?
BDA Food Factsheet: Vitamin D:
www.bda.uk.com/resource/covid-19-rapid-guideline-vitamin-d.html
NHS information on Vitamin D:
www.nhs.uk/conditions/vitamins-and-minerals/vitamin-d/
Vitamin D supplementation in winter:
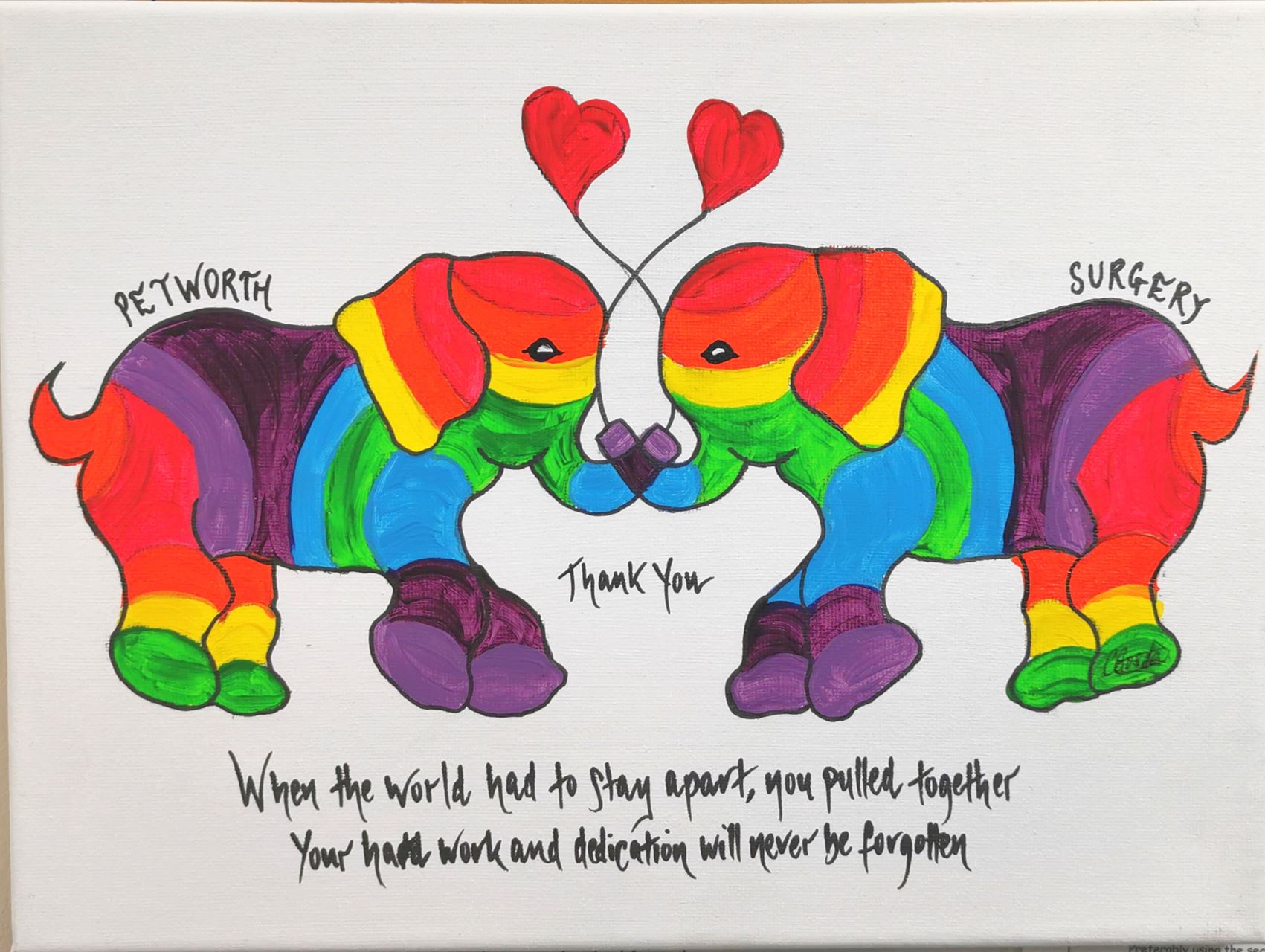
We received this beautiful canvas painting from a patient of the surgery.
Thank you Caroline! You have made our day!
You can find more of Caroline's art on her website: carolinegosdenart.com

Page created: 09 April 2020


